If your gums look swollen or bleed when you floss, you probably have some form of gum disease. You could have early signs of gingivitis. But how do you know when it turns into periodontitis? Knowing how to tell if you have gingivitis or periodontitis can guide you toward the best treatment options.
Gingivitis vs. Periodontitis
Gingivitis and periodontitis are different phases of gum disease, which can cause tooth loss. Unlike healthy gums that are pink and strong, diseased gums have plaque buildup containing inflammatory bacteria. The difference between periodontitis and gingivitis has to do with the progression of inflammation and infection.
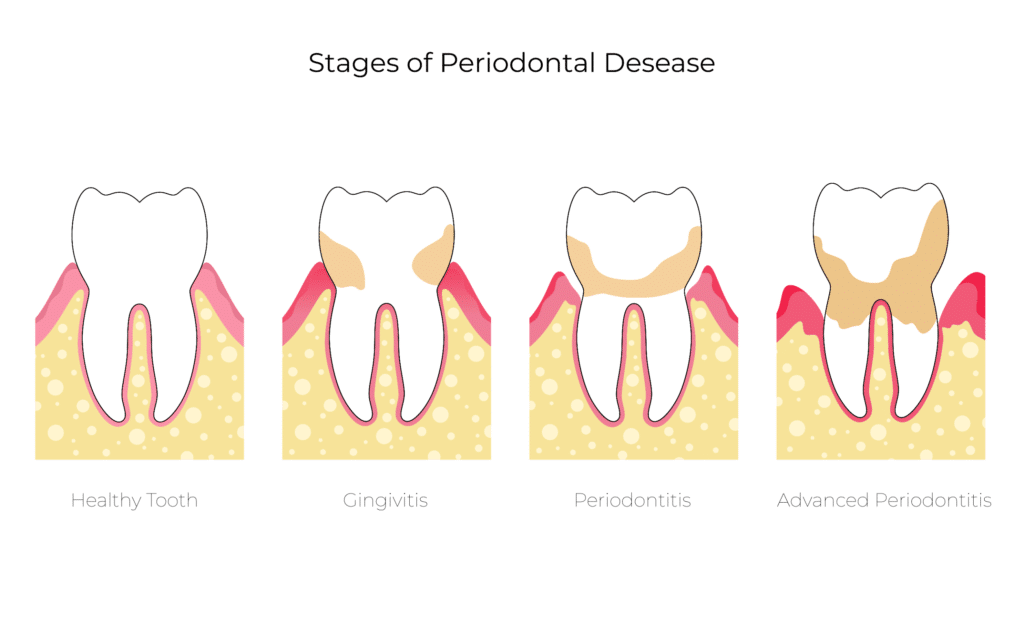
Gingivitis, the earliest stage of gum disease, derives from an increase of plaque leading to bacterial infection. With gingivitis, gums can get red, tender, and inflamed. They might also bleed during flossing or brushing.
Catching gingivitis early enough can help reverse some of the damage it causes. This is true when the disease has not yet impacted the bone and the tissue in which it rests.
Periodontitis represents the advanced stages of gum disease. Over 47% of adults over 30 in the United States experience chronic periodontitis. At this phase, the infection extends beyond the gums and causes the bones and connective tissues to degenerate. Symptoms of periodontitis include:
- Bad breath or foul taste
- Bleeding gums during brushing or flossing
- Gum recession
- Gums that are tender, red, or inflamed
- Inflammation in other parts of the body
- Pain while eating
- Teeth that move around or are loose
- Tooth loss
Treatments for Gingivitis and Periodontitis
See your dentist if you notice the signs of gum disease, no matter how minor they appear. It is possible to reverse gum disease with early detection and treatment.
Treating gum disease requires good oral hygiene every day. If you smoke, it is important that you stop or cut back. If your symptoms do not improve after professional cleanings, your dentist might prescribe an antibiotic as an antiseptic mouthwash, tablet, or gel.
Periodontal surgery might be required if gum disease does not subside with preventive care, professional cleanings, or antibiotics. If your dentist detects detached or receding gums, loose teeth, swelling, bleeding, or pain, they may recommend an intervention like scaling and root planing. During this procedure, the dentist uses a curette to scrape away plaque and tartar deep below the gum line. Then, the curette is used to smooth the roots to allow the reattachment of gums to the teeth.
Flap surgery involves lifting the gums back to allow for tartar and plaque removal. The dentist then sutures the gums together to fit around the tooth.
Your dentist or periodontist might recommend bone or gum grafting if bone or connective tissues are too damaged. With grafting, the dentist uses tissue or bone from other parts of the mouth for regeneration.
Preventing Gum Disease
The best line of defense against gingivitis and periodontitis is prevention. Consistent oral hygiene can go a long way to keeping gums healthy and warding off inflammation, infection, and tooth loss.
Brushing and Flossing
It is impossible to overstate the importance of brushing and flossing daily or after every meal. Regular brushing dislodges trapped food and keeps plaque from accumulating. The tongue needs brushing, too, because it can harbor infectious bacteria. Daily flossing is another crucial step in preventing gum disease because it removes particles a toothbrush cannot reach.
Smoking Cessation
Smoking is a risk factor for gum disease. Because smoking compromises your immune system, it can make it more difficult for the gums to fight off an infection or heal. If you do smoke, quit or consult your doctor for help quitting.
Fluoride Toothpaste
Fluoride provides a natural defense against tooth decay. Although most municipalities add fluoride to drinking water, it might not be enough to preserve oral health. Using toothpaste with fluoride can help prevent gum disease.
Therapeutic Mouthwash
As an added measure against plaque buildup, consider adding therapeutic mouthwash to your dental regimen. It is an over-the-counter product that can remove food particles, reduce plaque, and slow down tartar accumulation.
Make sure you use mouthwash as a supplement to—not a replacement for—brushing and flossing. As with all dental hygiene products, look for the American Dental Association’s (ADA) Seal of Acceptance to know it is effective and safe.
Regular Dental Cleanings and Checkups
You cannot get rid of tartar on your own, so twice-yearly professional cleanings and preventive care are necessary. In addition, regular dental checkups are essential to maintaining good oral health. During an office visit, your dentist will also check for signs of oral cancer, gum disease, and other dental ailments.
- Dental Implant Pros and Cons - August 26, 2023
- Receding Gums Stages - August 12, 2023
- When Is It Too Late for Gum Grafting? - July 8, 2023


